Editorial
| Rev Diabet Stud,
2008,
5(4):194-202 |
DOI 10.1900/RDS.2008.5.194 |
Gestational Diabetes: Pathogenesis and Consequences to Mother and Offspring
Risto Kaaja1,2, Tapani Rönnemaa2
1Department of Obstetrics and Gynecology, Helsinki University Hospital, Helsinki, Satakunta Central Hospital, Pori, Finland
2Department of Medicine, University of Turku and Turku University Hospital, Turku, Finland
Address correspondence to: Risto Kaaja, e-mail: risto.kaaja@utu.fi
Manuscript submitted February 1, 2009; resubmitted February 27, 2009; accepted February 28, 2009.
Keywords: gestational diabetes, insulin resistance, lifestyle intervention, risk factor, screening
Abstract
Gestational diabetes mellitus (GDM) is defined as glucose intolerance with onset or first recognition during pregnancy. Data from Western countries suggest that the prevalence of GDM is increasing, being almost 10% of pregnancies and probably reflecting the global obesity epidemic. The majority of women with GDM seem to have β-cell dysfunction that appears on a background of chronic insulin resistance already present before pregnancy. In less than 10% of GDM patients, defects of β-cell function can be due to autoimmune destruction of pancreatic β-cells, as in type 1 diabetes, or caused by monogenic mutations, as in several MODY subtypes. Diagnostic criteria for GDM vary worldwide and there are no clear-cut plasma glucose cut-off values for identifying women at a higher risk of developing macrosomia or other fetal complications. Because the oral glucose tolerance test (OGTT) is restricted to high risk individuals, 40% of GDM cases are left undiagnosed. Therefore, in high risk populations almost universal screening is recommended; only women considered to have very low risk do not need screening. Diet and exercise are the key elements in the treatment of GDM. If necessary, either insulin, certain oral hypoglycemic agents or combinations can be used to achieve normoglycemia. After delivery, women with GDM and their offspring have an increased risk for developing the metabolic syndrome and type 2 diabetes. Thus, pregnancy may act as a “stress test”, revealing a woman’s predisposition to T2D and providing opportunities for focused prevention of important chronic diseases.
Introduction
Gestational diabetes mellitus (GDM) is defined as glucose intolerance of variable severity with onset or first recognition during pregnancy [1]. Women with GDM represent a heterogeneous group. A proportion has unrecognized pre-existing non-insulin-dependent diabetes (type 2) and a small number has insulin-dependent type 1 diabetes, with onset during pregnancy.
The presence of GDM has implications for both the baby and the mother. Although there is no evidence that perinatal mortality increases in pregnancies with treated GDM, some studies have shown perinatal mortality increases in untreated GDM [2]. The characteristics of perinatal morbidity in children of GDM mothers are the same as for infants of mothers with overt diabetes (e.g., macrosomia, neonatal hypoglycemia, hyperbilirubinemia and respiratory distress syndrome) [3]. While considering longer term outcomes for the baby, evidence is gradually mounting that GDM adds an intrauterine environmental risk factor to an already increased genetic risk for the development of obesity and/or diabetes [4, 5]. For the mother, GDM is a strong risk factor for the development of permanent diabetes later in life (40% in 10 subsequent years) [6].
Obesity and prevalence of GDM
Women of reproductive age are commonly overweight and obese. For example, in the UK 32% of 35- to 64-year-old women are overweight and 21% are obese [7]. The trend towards weight gain among women of reproductive age is alarming. Between 1990 and 2000, the proportion of overweight among Finnish parturient women (BMI > 25) increased from 18.8% to 24.5% and the proportion of obese women (BMI > 30) increased from 7.5% to 11% [8]. Overweight prior to pregnancy, as well as inter-pregnancy weight gain, prediposes to various pregnancy complications, such as GDM [9, 10], with potentially serious long- and short-term health consequences for both mother and offspring. Data from Western countries suggest that the prevalence of GDM is increasing [11], likely reflecting the global obesity epidemic. In Finland already, up to 15% of women <45 years have elevated glucose levels during pregnancy [12]. By 2006, in Finland, the prevalence of GDM was prevalent in 8.5% of all pregnant women [13].
Pathogenetic mechanisms
Insulin resistance and relative pancreatic β-cell dysfunction
Insulin requirements are high during normal late pregnancy and differ only slightly between normal and gestational diabetic women. However, in contrast to healthy women, GDM women consistently show reduced insulin responses to nutrients [14, 15]. When insulin levels and responses are expressed relative to each individual’s degree of insulin resistance, a large defect in pancreatic β-cell function is consistently found in women with prior GDM [16]. The majority of women with GDM appear to have β-cell dysfunction that occurs on a background of chronic insulin resistance already present before pregnancy [17, 18]. Both lean and obese women developing GDM show distinct resistance to the ability of insulin to stimulate glucose disposal and to suppress both glucose production and fatty acid levels [14, 19].
Defects in the binding of insulin to its receptor in skeletal muscle do not appear to be involved in the state of insulin resistance in GDM women [20]. Many other defects, such as alterations in the insulin signaling pathway, reduced expression of PPARγ and reduced insulin-mediated glucose transport have been found in skeletal muscle or fat cells of women with GDM [21]. Whether any of these defects are primary or the result of more fundamental defects in insulin action is currently unknown. It has recently been suggested that post-receptor defects are present in the insulin signaling pathway in the placenta of women with pregnancies complicated by diabetes and obesity. In addition, expression studies demonstrate that post-receptor alterations in insulin signaling may be under selective maternal regulation and are not regulated by the fetus [22].
On the other hand, recently, it has also been proposed that events leading to the development of GDM are triggered by an antigenic load which is the fetus itself. Human leukocyte antigen-G (HLA-G) expression, which functions to protect the fetus from immune attack by down-regulating cytotoxic T cell responses to fetal trophoblast antigens, is postulated to protect pancreatic islet cells as well. The interaction between HLA-G and nuclear factor-κB (NF-κB) is suggested to be central in the events leading to GDM development. It has been postulated that the development of DM in patients who have undergone organ transplantation is analogous to GDM development in a proportion of pregnancies. In both cases, an antigenic load triggers the diabetogenic process. If future studies further support this hypothesis then it may be possible to use recombinant HLA-G for the prevention of GDM in high risk patients [23].
Rare causes for GDM
In GDM women, defects in β-cell function can also be due to autoimmune destruction of pancreatic β-cells, as in type 1 diabetes. This is characterized by circulating immune markers directed against pancreatic islets (anti-islet cell antibodies) or β-cell antigens (such as glutamic acid decarboxylase, GAD, or insulin autoantibodies, IAA). These patients appear to have evolving type 1 diabetes. This is usually diagnosed through routine glucose screening during pregnancy. Anti-islet cell or anti-GAD antibodies are present in less than 10% of GDM patients, who are not always lean. These women can rapidly develop overt diabetes after pregnancy [21, 24].
Another cause for a defective β-cell function in GDM are mutations in autosomes (autosomal dominant inheritance pattern, commonly referred to as maturity-onset diabetes of the young (MODY), with genetic subtypes denoted as MODY-1, MODY-2, etc.). Mutations that cause several subtypes of MODY have been found in women with GDM. These include mutations in genes coding for: (a) glucokinase (MODY-2), (b) hepatocyte nuclear factor 1α (MODY-3), (c) and insulin promoter factor 1 (MODY-4) [21, 25]. Together, these monogenic forms of GDM account for less than 10% of al GDM cases [21]. They likely represent cases of symptomless preexisting diabetes that are first detected by routine glucose screening during pregnancy.
How to diagnose GDM
There has been much debate about whether universal or selective screening of pregnant women for GDM is more appropriate. Selective screening for those with the highest risk has been recommended especially in low risk countries. Risk factors for GDM include:
- Glucosuria
- Age over 30 years
- Obesity
- Family history of diabetes
- Past history of GDM or glucose intolerance
- Previous macrosomic child
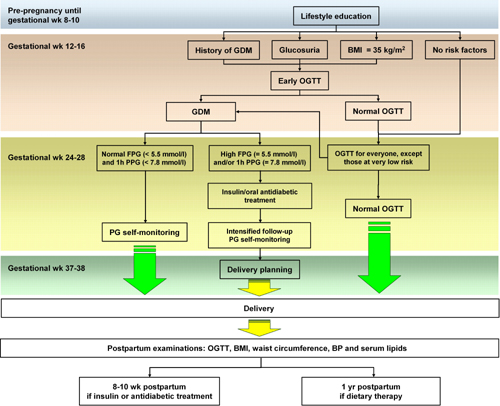
However, as the prevalence of GDM increases, there is a tendency towards universal screening, because about 40% of GDM cases have previously been left undiagnosed, due to the glucose challenge test being restricted to high risk individuals [26, 27]. The Finnish current guidelines [13] and the Australasian Diabetes in Pregnancy Society (ADIPS) [2] recommend that screening for GDM should be considered in all pregnant women. There are only a few exceptions for whom an oral glucose tolerance test (OGTT) is not indicated. These are very low risk patients, including 1. nulliparous women < 25 years of age and BMI < 25 kg/m2, 2. multiparous women < 40 years of age and BMI < 25 kg/m2 and who have had no previous macrosomic children (Figure 1) [2, 28-31].
 |
 |
Figure 1. Guideline for the supervision of pregnancy with regard to gestational diabetes mellitus (GDM). Pregnant women (except for those at very low risk) should be screened for GDM in gestational wk 24-28. Early oral glucose tolerance test (OGTT) should be carried out in gestational wk 12-16 in cases of existing risk factors. If GDM is diagnosed, treatment should be carried out based on fasting plasma glucose (FPG) and postprandial plasma glucose (PPG) values. Insulin and/or oral antidiabetic therapy in addition to intensive control of PG and delivery planning should be considered in cases of high FPG and 1h PPG. Postpartum follow-up examinations should include OGTT, body mass index (BMI), waist circumference, blood pressure (BP) and serum lipids. The examinations should take place so much earlier the more intensive was the treatment of GDM during pregnancy. It can be as recently as one year postpartum, if only dietary therapy was carried out during pregnancy. If the woman has been treated with insulin or antidiabetic agents during pregnancy, then examination should take place 8-12 weeks postpartum. If the first follow-up was normal, subsequent follow-ups in 1-3 year intervals. Figure modified from Finnish current guidelines for the treatment of gestational diabetes, 2008 [13]. |
|
GDM is generally diagnosed using a two-hour OGTT with a 75 g dose of glucose. There is significant variation between the criteria for determining abnormal values (Table 1). Diagnosis is generally based on one or more abnormal values in the test. The most frequently used diagnostic pathological values for plasma glucose concentrations are ≥ 5.3 mmol/l after fasting, ≥ 10.0 mmol/l after 1 hour and ≥ 8.6 mmol/l after 2 hours from the start of the test. OGTT is usually performed between the 24th and 28th week of pregnancy. However, it is recommended that OGTT is performed earlier, between the 12th and 16th week of pregnancy, if the risk of gestational diabetes is estimated to be high. These high risk cases include: 1. mothers with severe obesity in early pregnancy (BMI > 35 kg/m2), 2. GDM occurred in a previous pregnancy, 3. a strong family history of diabetes, 4. glucosuria (Figure 1).
Table
1.
Recommendations on diagnostic criteria for GDM by a 75 g oral glucose tolerance test |
|
 |
 |
Legend:
NDDG: National Diabetes Data Group. |
|
Outcome of pregnancy complicated by GDM
The outcome of pregnancy among mothers with GDM is still worse than that of non-diabetic women. GDM is associated with a significantly increased risk of macrosomia, shoulder dystocia, birth injuries as well as neonatal hypoglycemia and hyperbilirubinemia [3, 27]. Even border-line GDM has been linked with an increased frequency of perinatal complications [32]. Women with GDM also have higher rates of caesarean sections and induced deliveries [3]. The HAPO Study Cooperative Research Group recently showed a strong and continuous correlation between maternal glucose levels (even below the values diagnostic of GDM) and increased birth weight and cord-blood serum C-peptide levels [33]. GDM increases the offspring’s predisposition to obesity and diabetes [27]. GDM and fetal macrosomia also significantly increase the child’s risk of developing the metabolic syndrome in childhood [34].
In a recently published study, 63 Chinese children, whose mothers had GDM during pregnancy, were followed until the age of 8 (median), together with 101 control children, whose mothers had normal glucose tolerance during pregnancy. After adjustment for gender and age, children exposed to maternal GDM had significantly higher systolic and diastolic BP, and lower high-density lipoprotein cholesterol. A high umbilical cord insulin level at birth was associated with abnormal glucose tolerance in the offspring. Thus, maternal GDM increases the offspring’s cardiometabolic risk. In utero hyperinsulinemia is an independent predictor of abnormal glucose tolerance in childhood [35].
Roughly 10-30% of women with GDM develop pre-eclampsia (PE), another serious pregnancy disorder [36, 37]. The incidence of PE among GDM mothers increases with both the severity of GDM and the pre-pregnancy BMI [37]. PE predisposes the patient to perinatal complications such as perinatal death, prematurity and intrauterine growth retardation [37]. In GDM, concurrent pregnancy-induced hypertension further increases the adverse outcomes [38].
The effects of GDM for the mother
For the mother, GDM is a sign of increased risk of developing overt diabetes. The pathogenesis of the most common type of GDM is similar to that of type 2 diabetes (T2D), with both pancreatic β-cell dysfunction and chronic insulin resistance playing decisive roles [27]. Pregnancy as an insulin resistant state may reveal even the smallest pre-existing defects in insulin secretion or insulin sensitivity and as a consequence, relative β-cell failure appears [7]. Up to 10% of patients with prior GDM are diagnosed with T2D soon after delivery and, during a ten-year follow-up, the risk of developing T2D is approximately 40% [6]. The cumulative incidence of T2D is highest in the first 5 years after pregnancy and then it decreases, reaching a plateau at ten years postpartum [39]. After delivery, women with GDM often have an increased risk for metabolic syndrome, and shortly after delivery these women have been shown to express early markers of vascular diseases such as disturbed endothelial function and increased intima-media thickness of carotid arteries [40]. Thus, pregnancy may act as a "stress test", revealing a woman's predisposition to T2D and providing opportunities for focused prevention of important chonic diseases [41].
There is a high risk that a woman develop T2D after pregnancy complicated by GDM. How can this risk be estimated? This is perhaps not so relevant as the risk is anyhow high. Small studies have detected increased circulating levels of leptin and inflammatory markers TNF-α and C-reactive protein, as well as decreased levels of adiponectin in women with prior GDM. Increased fat content in liver and muscle has also been reported in women with previous GDM [21]. All of these findings are consistent with the current understanding of some potential causes of obesity-related insulin resistance.
Prevention of gestational diabetes
Prevention of obesity is of utmost importance in the prevention of GDM. A retrospective UK study of 287,213 pregnancies between 1989 and 1997 showed that after adjusting for ethnic group, parity, maternal age and history of hypertension, women with a BMI ≥ 30 were more likely to develop gestational diabetes than women with a BMI of 20.0-24.9 (OR 3.65, 95% CI 3.25-3.98) [9]. These findings were similar to a later Australian study of 14,230 pregnancies which showed that the odds (corrected for maternal age, parity, ethnicity, educational and smoking status) of developing GDM was 2.95 times higher (95% CI 2.05-4.25) in obese women (BMI 30.01-40.00) compared with normal-weight (BMI 20.01-25.00) women [42].
Weight loss before conception through dietary modification
A weight loss of 4.5 kg between pregnancies has been shown to reduce the risk of developing GDM in a subsequent pregnancy by up to 40% [42]. A 10% weight loss over six months is suggested to be an ideal amount, which is safe and possible [42]. It has been suggested that weight loss regimens in the first trimester of pregnancy may increase the risk of fetal neural tube defects, although this finding does not appear to be associated with weight loss prior to pregnancy [43].
Regular moderate-intensity physical activity
Exercise has been found to be helpful in improving glycemic control in women with GDM and may play a role in its prevention [44]. Regular exercise and a healthy diet facilitate weight control and improve insulin sensitivity. Exercise and weight loss decrease sympathetic activity and/or increase parasympathetic activity as well as lower resting heart rate and blood pressure [45, 46]. It seems possible that improving insulin sensitivity and reducing sympathetic overactivity in high-risk women with regular exercise and weight loss may reduce the risk of GDM and PE. Lifestyle interventions have been shown to prevent the onset of T2D in overweight subjects with impaired glucose tolerance [47, 48]. Although studies investigating exercise and diet interventions aimed at GDM/PE prevention have not yet been conclusive [49], the results of preliminary cohort and case-control studies look promising. The risk of GDM is inversely proportional to the degree of physical activity in the year prior to pregnancy [50]. Exercise before and during early pregnancy is associated with 51% and 48% reductions in GDM risk, respectively [51]. Exercise started before and continued throughout pregnancy may lead to GDM and PE risk reductions of 69% and 40%, respectively [52].
Management of GDM
A team approach is ideal for managing women with GDM and, if available, should be used. The team should usually comprise an obstetrician, diabetes physician, a diabetes educator (diabetes midwifery educator), a nutritionist, a midwife and a pediatrician. In practice, however, it is not always possible to employ a team due to limited resources. In such circumstances, management by an obstetrician or obstetric general practitioner knowledgeable in GDM management, often with the assistance of an appropriately skilled nutritionist, diabetes educator or midwife, is acceptable.
Dietary therapy
Dietary therapy is the primary therapeutic strategy for the achievement of acceptable glycemic control in GDM. All women should receive nutritional advice, preferably from an appropriately skilled dietitian. The American Diabetes Association and the American College of Obstetrics and Gynecology recommend nutrition therapy for GDM that emphasizes food choices to promote appropriate weight gain and normoglycemia without ketonuria, and moderate energy restriction for obese women. However, it is important to avoid a pronounced calorie-restricted diet, as this can predispose the patient to ketonuria, and lead to the birth of infants that are small for their gestational age (SGA). SGA children carry the increased risk of developing diabetes in later life [53-55]. Currently, due to a lack of large randomized trials, there is no firm scientific basis for recommendations of how dietary composition, i.e. amounts and types of carbohydrates and fats, should be modified in patients with GDM. Recently, moderate exercise has been recognized as an adjunct therapy, with potential benefits when used together with diet or diet and insulin therapy, in the management of GDM in women without a medical or obstetric contraindication [56].
Glycemic control
Glycemic control needs to be monitored and self-monitoring of blood glucose levels is the optimal method and is well tolerated by most women. On initiation of self-monitoring at least one fasting and one 1 hour postprandial glucose level should be obtained daily. The frequency may change depending on the results of blood glucose monitoring and the progression of the pregnancy. If self-monitoring is not possible, fasting and 1 hour postprandial laboratory capillary blood or venous plasma glucose levels should be performed regularly (at 1 to 2 weekly intervals). In pregnancies complicated by GDM, the value of self-monitoring of blood glucose and appropriate insulin therapy in the prevention of macrosomia and its associated perinatal complications has been demonstrated [27]. The minimum goals for glycemic control are [57]:
- A fasting capillary (venous plasma) blood glucose level <5.5 mmol/l
- An 1 hour postprandial capillary (venous plasma) blood glucose level <8.0 mmol/l
Langer and Hod support the recommended fasting glycemia goal of <5.5 mmol/l [58]. The authors have shown that the rates of large-for-gestational-age (LGA) infants increase in diet-treated GDM pregnant women if the fasting glucose level is between 5.3 and 5.8 mmol/l (LGA prevalence 28.6%) compared with those with a level below 5.3 mmol/l (LGA prevalence 5.35%) [58]. Insulin treatment was shown to reduce the rate of LGA infants to 10.3% in GDM pregnancies with pretreatment fasting glucose levels between 5.3 and 5.8 mmol/l [58]. HbA1c levels may be used as an ancillary test, as assurance that the self-monitored blood glucose results are appropriate. Fructosamine concentration, adjusted for plasma protein levels, reflects average glycemia during the previous two weeks. This is a shorter time period than that reflected by the HbA1c test. It is therefore used in some countries during pregnancy. However, HbA1c or fructosamine can by no means substitute for self-monitoring of blood glucose [42]. Continuous glucose monitoring (CGM) may reveal high postprandial peaks not necessarily observable with self-monitoring of glucose but at present CGM is not recommended for routine use in guiding GDM treatment [59, 60].
Insulin therapy
Insulin therapy should be considered if the plasma glucose goals are not met on two or more occasions during a 1 to 2 week follow-up, particularly if there is clinical or ultrasonographic suspicion of macrosomia. However, the benefit of instituting insulin therapy after 38 weeks of gestation is unproven.
Human insulin and insulin analogues such as insulin lispro, aspart insulin and glargine can be used. They have been shown to be safe mainly in type 1 diabetic women, but they are also used in women with GDM. The doses may be higher than those required in non-pregnant subjects and should be reviewed frequently so that adequate glycemic control is achieved rapidly. Care should be taken to minimize the risk of hypoglycemia, especially nocturnal episodes [61, 62].
The ACHOIS trial was a landmark study. It showed that the rate of serious perinatal complications was significantly lower among the infants of 490 women, who received dietary advice, blood glucose monitoring, and insulin therapy as needed (the "intervention" group), than among the infants of 510 women in the routine-care group (1 percent vs. 4 percent, p = 0.01) [63].
Oral hypoglycemic agents
Oral hypoglycemic agents (glyburide and metformin) have been shown to be a possible alternative to insulin in the medical treatment of GDM [64-66]. Recently a systematic review of randomized controlled trials and observational studies of maternal and neonatal outcomes in women with GDM was conducted [67]. Women treated with oral hypoglycemic agents were compared with those treated with all types of insulin. Two trials compared insulin to glyburide; one trial compared insulin, glyburide, and acarbose; and one trial compared insulin to metformin. No significant differences were found in maternal glycemic control or cesarean delivery rates between the insulin and glyburide groups. A meta-analysis showed similar infant birth weights between women treated with glyburide and women treated with insulin (mean difference -93 g, 95% -191 to 5 g). There was a higher proportion of infants with neonatal hypoglycemia in the insulin group (8.1%) compared with the metformin group (3.3%) (p = 0.008). No substantial maternal or neonatal outcome differences were found with the use of glyburide or metformin compared with use of insulin in women with GDM. But it should be noticed that in 20% to 50% of cases in these trials the oral therapy seemed to be insufficient and additional insulin was needed to achieve the glycemic goals [64]. In addition, until now there has not been sufficient long-term follow-up data on the safety of metformin use in GDM with respect to the physical and psychological health of the offspring.
Conclusions
GDM has implications for both the baby and the mother. There is no evidence that the rate of perinatal mortality increases in pregnancies with treated GDM but some studies have shown perinatal mortality to increase in untreated GDM. The diagnostic criteria for GDM vary worldwide and there are no clear-cut plasma glucose cut-off values for indicating higher risk for macrosomia or other fetal complications. Diet and exercise are the key elements in the treatment of GDM. If necessary, insulin and possibly certain oral hypoglycemic agents, separately or combined with insulin, can be used to achieve normoglycemia.
After delivery, women with GDM often have an increased risk for developing the metabolic syndrome and early markers of vascular diseases such as disturbed endothelial function and increased intima-media thickness of carotid arteries. Thus, pregnancy may act as a "stress test", revealing a woman's predisposition to T2D and providing opportunities for focused prevention of important chronic diseases. Prevention of GDM by lifestyle changes should be attempted as it could ensure a healthier future for the child and the mother. No large, randomized controlled intervention trials have yet tested the effect of lifestyle changes in the prevention of GDM and its complications. More studies are required to define the role of antihyperglycemic agents other than insulin in the treatment of GDM that does not respond sufficiently to lifestyle intervention.
References
- Metzger BE. Proceedings of the third international workshop-conference on gestational diabetes mellitus. Diabetes 1991. 40(Suppl 2):1-201. [DOD]
- Hoffman L, Nolan C, Wilson JD, Oats JJ, Simmons D. Gestational diabetes mellitus - management guidelines. The Austalasian Diabetes in Pregnancy Society. Med J Aust 1998. 169(2):93-97. [DOD]
- Hod M, Merlob P, Friedman S, Schoenfeld A, Ovadia J. Gestational diabetes mellitus: a survey of perinatal complications in the 1980s. Diabetes 1991. 40(Suppl 2):74-78. [DOD]
- Van Assche FA, Aerts L, Holemans K. The effects of maternal diabetes on the offspring. Baillieres Clin Obstet Gynaecol 1991. 5(2):485-492. [DOD] [CrossRef]
- Silverman BL, Metzger BE, Cho NH, Loeb CA. Impaired glucose tolerance in adolescent offspring of diabetic mothers: relationship to fetal hyperinsulinism. Diabetes Care 1995. 18:611-617. [DOD] [CrossRef]
- Lauenborg J, Hansen T, Jensen DM, Vestergaard H, Mølsted-Pedersen L, Hornnes P, Locht H, Pedersen O, Damm P. Increasing incidence of diabetes after gestational diabetes: a long-term follow-up in a Danish population. Diabetes Care 2004. 27:1194-1199. [DOD] [CrossRef]
- Yu CK, Teoh TG, Robinson S. Obesity in pregnancy. BJOG 2006. 113(10):1117-1125. [DOD] [CrossRef]
- Raatikainen K, Heiskanen N, Heinonen S. Transition from overweight to obesity worsens the pregnancy outcome in a BMI-dependent manner. Obesity (Silver Spring) 2006. 14(1):165-171. [DOD] [CrossRef]
- Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, Regan L, Robinson S. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord 2001. 25(8):1175-1182. [DOD] [CrossRef]
- Villamor E, Cnattingius S. Interpregnancy weight change and risks of adverse pregnancy outcomes: a population-based study. Lancet 2006. 368:1164-1170. [DOD] [CrossRef]
- Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS. Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care 2005. 28(3):579-584. [DOD] [CrossRef]
- Kaaja R, Luoto R. Complications of pregnancy. In: Koponen P, Luoto R (eds.). Reproductive health in Finland. The Health 2000 Study. Publications of the National Public Health Institute B5/2004. [DOD]
- Working group on gestational diabetes. National guidelines for gestational diabetes. Duodecim 2008. 124:1556-1569. [DOD]
- Catalano PM, Huston L, Amini SB, Kalhan SC. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes. Am J Obstet Gynecol 1999. 180:903-916. [DOD] [CrossRef]
- Homko C, Sivan E, Chen X, Reece EA, Boden G. Insulin secretion during and after pregnancy in patients with gestational diabetes mellitus. J Clin Endocrinol Metab 2001. 86(2):568-573. [DOD] [CrossRef]
- Buchanan TA. Pancreatic B-cell defects in gestational diabetes: implications for the patogenesis and prevention of type 2 diabetes. J Clin Endocrinol Metab 2001. 86(3):989-993. [DOD] [CrossRef]
- Damm P, Vestergaard H, Kuhl C, Pedersen O. Impaired insulin-stimulated nonoxidative glucose metabolism in glucose-tolerant women with previous gestational diabetes. Am J Obstet Gynecol 1996. 174:722-729. [DOD] [CrossRef]
- Kautzky-Willer A, Prager R, Waldhausl W, Pacini G, Thomaseth K, Wagner OF, Ulm M, Streli C, Ludvik B. Pronounced insulin resistance and inadequate betacell secretioncharacterize lean gestational diabetes during and after pregnancy. Diabetes Care 1997. 20:1717-1723. [DOD] [CrossRef]
- Xiang AH, Peters RK, Trigo E, Kjos SL, Lee WP, TA Buchanan TA. Multiple metabolic defects during late pregnancy in women at high risk for type 2 diabetes mellitus. Diabetes 1999. 48:848-854. [DOD] [CrossRef]
- Damm P, Handberg A, Kühl C, Beck-Nielsen H, Mølsted-Pedersen L. Insulin receptor binding and tyrosine kinase activity in skeletal muscle from normal pregnant women and women with gestational diabetes. Obstet Gynecol 1993. 82(2):251-259. [DOD]
- Buchanan TA, Xiang AH. Gestational diabetes mellitus. J Clin Invest 2005. 115(3):485-491. [DOD]
- Colomiere M, Permezel M, Riley C, Desoye G, Lappas M. Defective insulin signalling in placenta from pregnancies complicated by gestational diabetes mellitus. Eur J Endocrinol 2009. In press. [DOD]
- Oztekin O. New insights into the pathophysiology of gestational diabetes mellitus: possible role of human leukocyte antigen-G. Med Hypotheses 2007. 69(3):526-530. [DOD] [CrossRef]
- Catalano PM, Tyzbir ED, Sims EA. Incidence and significance of islet cell antibodies in women with previous gestational diabetes. Diabetes Care 1990. 13:478-482. [DOD] [CrossRef]
- Ellard S, Beards F, Allen LL, Shepherd M, Ballantyne E, Harvey R, Hattersley AT. A high prevalence of glucokinase mutations in gestational diabetic subjects selected by clinical criteria. Diabetologia 2000. 43:250-253. [DOD] [CrossRef]
- Poyhonen-Alho MK, Teramo KA, Kaaja RJ, Hiilesmaa VK. 50gram oral glucose challenge test combined with risk factor-based screening for gestational diabetes. Eur J Obstet Gynecol Reprod Biol 2005. 121(1):34-37. [DOD] [CrossRef]
- Griffin ME, Coffey M, Johnson H, Scanlon P, Foley M, Stronge J, O'Meara NM, Firth RG. Universal vs. risk factor-based screening for gestational diabetes mellitus: detection rates, gestation at diagnosis and outcome. Diabet Med 2000. 17(1):26-32. [DOD] [CrossRef]
- O'Sullivan JB, Mahan CM. Criteria for the oral glucose tolerance test in pregnancy. Diabetes 1964. 13:278-285. [DOD]
- National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 1979. 28(12):1039-1057. [DOD]
- Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 1982. 144:768-773. [DOD]
- World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Report of a WHO consultation 1999. WHO/NCD/NCS/99.2. [DOD]
- Ju H, Rumbold AR, Willson KJ, Crowther CA. Borderline gestational diabetes and pregnancy outcomes. BMC Pregnancy Childbirth 2008. 8:31. [DOD] [CrossRef]
- HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, McIntyre HD, Oats JJ, Persson B, Rogers MS, Sacks DA. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008. 358(19):1991-2002. [DOD] [CrossRef]
- Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity and gestational diabetes. Pediatrics 2005. 115(3):E290-E296. [DOD] [CrossRef]
- Tam WH, Yang X, Ko GT, Tong PC, Cockram CS, Sahota DS, Rogers MS, Chan JC. Glucose intolerance and cardiometabolic risk in children exposed to maternal gestational diabetes mellitus in utero. Pediatrics 2008. 122:1229-1234. [DOD] [CrossRef]
- Montoro MN, Kjos SL, Chandler M, Peters RK, Xiang AH, Buchanan TA. Insulin resistance and preeclampsia in gestational diabetes mellitus. Diabetes Care 2005. 28:1995-2000. [DOD] [CrossRef]
- Roberts JM, Redman CW. Pre-eclampsia: more than pregnancy-induced hypertension. Lancet 1993. 341:1447-1451. [DOD] [CrossRef]
- Yogev Y, Xenakis EM, Langer O. The association between preeclampsia and the severity of gestational daibetes: the impact of glycemic control. Am J Obstet Gyn 2004. 191:1655-1660. [DOD] [CrossRef]
- Kim C, Neston K, Knopp R. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 2002. 25:1862-1868. [DOD] [CrossRef]
- Bo S, Valpreda S, Menato G, Bardelli C, Botto C, Gambino R, Rabbia C, Durazzo M, Cassader M, Massobrio M, Pagano G. Should we consider gestational diabetes a vascular risk factor? Atherosclerosis 2007. 194:E72-E79. [DOD]
- Kaaja RJ, Greer IA. Manifestation of chronic disease during pregnancy. JAMA 2005. 294(21):2751-2157. [DOD] [CrossRef]
- Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an Australian obstetric population. Med J Austr 2006. 184:56-59. [DOD]
- Carmichael SL, Shaw GM, Schaffer DM, Laurent C, Selvin S. Dieting behaviors and risk of neural tube defects. Am J Epidemiol 2003. 158:1127-1131. [DOD] [CrossRef]
- Bung P, Artal R, Khodiguian N. Regular exercise therapy in disorders of carbohydrate metabolism in pregnancy--results of a prospective, randomized longitudinal study. Geburtshilfe Frauenheilkd 1993. 53(3):188-193. [DOD] [CrossRef]
- Zanesco A, Antunes E. Effects of exercise training on the cardiovascular system: Pharmacological approaches. Pharmacol Ther 2007. 114:307-317. [DOD] [CrossRef]
- van Baak MA. The peripheral sympathetic nervous system in human obesity. Obes Rev 2001. 2:3-14. [DOD] [CrossRef]
- Lee S, Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Graham TE, Ross R. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without type 2 diabetes. J Appl Physiol 2005. 99(3):1220-1225. [DOD] [CrossRef]
- Pitsavos C, Panagiotakos D, Weinem M, Stefanadis C. Diet, exercise and the metabolic syndrome. Rev Diabet Stud 2006. 3(3):118-126. [DOD] [CrossRef]
- Meher S, Duley L. Exercise or other physical activity for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev 2006. 2:CD005942. [DOD]
- Rudra CB, Williams MA, Lee IM, Miller RS, Sorensen TK. Perceived exertion in physical activity and risk of gestational diabetes mellitus. Epidemiology 2006. 17:31-37. [DOD] [CrossRef]
- Dempsey JC, Butler CL, Sorensen TK, Lee IM, Thompson ML, Miller RS, Frederick IO, Williams MA. A case-control study of maternal recreational physical activity and risk of gestational diabetes mellitus. Diabetes Res Clin Pract 2004. 66:203-215. [DOD] [CrossRef]
- Dempsey JC, Butler CL, Williams MA. No need for a pregnant pause: physical activity may reduce the occurrence of gestational diabetes and pre-eclampsia. Exerc Sport Sci Rev 2005. 33:141-149. [DOD] [CrossRef]
- Knopp RH, Magee MS, Raisys V, Benedetti T, Bonet B. Hypocaloric diets and ketogenesis in the management of obese gestational diabetic women. J Am Coll Nutr 1991. 10(6):649-667. [DOD]
- Geremia C, Cianfarani S. Insulin sensitivity in children born small for gestational age (SGA). Rev Diabet Stud 2004. 1(2):58-65. [DOD] [CrossRef]
- Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidemia (syndrome X): relation to reduced fetal growth. Diabetologia 1993. 36:62-67. [DOD] [CrossRef]
- Royal College of Obstetricians and Gynaecologists. Exercise in Pregnancy. Statement no 4, London, 2006. Available online at http://www.rcog.org.uk/files/rcog-corp/uploaded-files/RCOGStatement4ExercisePregnancy2006.pdf, accessed February 2009. [DOD]
- Simmons DS, Walters BN, Wein P, Cheung NW, Australasian Diabetes in Pregnancy Society. Guidelines for the management of gestational diabetes mellitus revisited. Med J Aust 2002. 176(7):352. [DOD]
- Langer O, Hod M. Management of gestational diabetes mellitus. Obstet Gynecol Clin North Am 1996. 23(1):137-159. [DOD] [CrossRef]
- Kestila KK, Ekblad UU, Rönnemaa T. Continuous glucose monitoring versus self-monitoring of blood glucose in the treatment of gestational diabetes mellitus. Diabetes Res Clin Pract 2007. 77:174-179. [DOD] [CrossRef]
- Yogev Y, Hod M. Use of new technologies for monitoring and treating diabetes mellitus. Obstet Gynecol Clin North Am 2007. 34(2):241-253. [DOD] [CrossRef]
- Singh C, Jovanovic L. Insulin analogues in the treatment of diabetes in pregnancy. Obstet Gynecol Clin North Am 2007. 34(2):275-291. [DOD] [CrossRef]
- Imbergamo MP, Amato MC, Sciortino G, Gambina M, Accidenti M, Criscimanna A, Giordano C, Galluzzo A. Use of glargine in pregnant women with type 1 diabetes mellitus: a case-control study. Clin Ther 2008. 30(8):1476-1484. [DOD] [CrossRef]
- Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Eng J Med 2005. 352(24):2477-2486. [DOD] [CrossRef]
- Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Eng J Med 2000. 343:1134-1138. [DOD] [CrossRef]
- Rowan JA, Hague WM, Gao W, Battin MR, Moore MP, Mig Trial Investigators. Metformin versus insulin for the treatment of gestational diabetes. N Eng J Med 2008. 358(19):2003-2015. [DOD] [CrossRef]
- Tertti K, Ekblad U, Vahlberg T, Rönnemaa T. Comparison of metformin and insulin in the treatment of gestational diabetes: A retrospective, case-control study. Rev Diabet Stud 2008. 5(2):95-101. [DOD] [CrossRef]
- Nicholson W, Bolen S, Witkop CT, Neale D, Wilson L, Bass E. Benefits and risks of oral diabetes agents compared with insulin in women with gestational diabetes: a systematic review. Obstet Gynecol 2009. 113:193-205. [DOD]
This article has been cited by other articles:
|